Menopause brings a drop in estrogen that often causes vaginal tissue changes. The condition is sometimes called Genitourinary Syndrome of Menopause (GSM), and it makes the vaginal lining thinner, drier, and more fragile. Common symptoms include vaginal dryness, burning, itching, and pain with sex. In fact, the Cleveland Clinic notes that “the lining of your vagina gets drier and thinner from a lack of estrogen. Burning, itching, spotting, and pain with sex are common symptoms”. These changes often require targeted care, since, unlike hot flashes, Menopause Vaginal Itching usually worsen over time without treatment.
Understanding Menopause and Vaginal Itching
Menopause is defined as the end of menstrual periods, usually occurring in a woman’s early 50s. It triggers major hormonal shifts – especially a sharp fall in estrogen – that can affect many body systems. The vagina and vulva have estrogen receptors, so low estrogen causes the tissues to become thin, dry, and irritated. As a result, many women experience vaginal itching (medically called vulvar pruritus) around menopause. This itching often goes along with vaginal dryness, since less estrogen means less natural lubrication.
Vaginal itching during menopause may feel like an uncomfortable, persistent urge to scratch the skin of the vagina or vulva. Because the skin is thinner and more delicate, even minor friction (such as tight clothing) or irritants can trigger itchiness. In some cases, microscopic tears from dryness can even let bacteria in, raising the risk of infections that further irritate the area. These symptoms are all part of GSM – a cluster of genital-urinary changes that can include vaginal itching, burning, and discomfort. Understanding that itching is a symptom of menopause not a permanent condition, can help women seek the right relief.
Why Hormonal Changes Cause Vaginal Discomfort
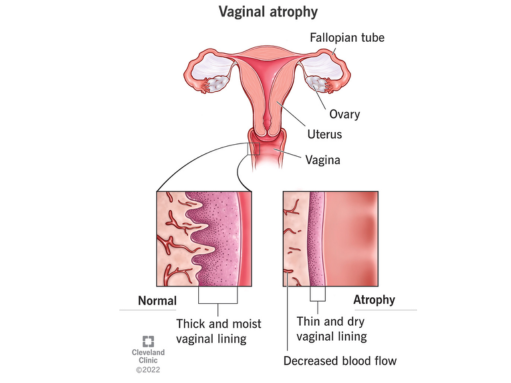
The key culprit is hormonal imbalance: when ovarian estrogen levels fall, vaginal tissues lose thickness and moisture. Mayo Clinic explains that lower estrogen causes the tissues in the vagina to become thinner, drier, less elastic, and more fragile. This is why a lack of estrogen during menopause is the main reason for vaginal discomfort. The normal healthy vaginal lining is several layers thick and well-hydrated; without estrogen, it becomes “thin and dry,” as shown in medical diagrams.
Lower estrogen levels also mean the vagina’s pH can rise (becoming less acidic), disrupting the natural balance of bacteria. These changes reduce natural lubrication and blood flow, contributing to vaginal dryness, itching, and irritation. Over time, untreated dryness and thinning can even make sex painful or painful urination more common. In short, the hormonal changes of menopause directly cause vaginal itching and discomfort – it’s not “just in your head,” but a well-documented effect of estrogen loss.
Common Symptoms: Vaginal Dryness, Irritation, and Skin Changes
Typical symptoms of menopause-related vaginal changes include:
- Vaginal dryness and lack of lubrication: The vagina produces less natural moisture, leading to a persistently dry feeling. Mayo Clinic notes that GSM symptoms can include “Dryness, burning or itching in the vagina”. Women may feel the vagina is dry even when not sexually aroused.
- Itching and irritation: Often called vulvar pruritus, this itchiness can affect the vulva (outer vagina) and the vaginal walls. It typically worsens if the skin is rubbed. The Menopause Society confirms that burning, itching, or irritation of the vulva and vagina are common GSM symptoms.
- Pain or discomfort, especially during sex: With thinning tissues and less lubrication, sex can become painful (dyspareunia). The vagina may feel tighter or less elastic. Menopause.org explains that “dryness and thinning of the vagina… is the most common cause of painful sex at midlife”. Small tears or bleeding can occur, further irritating the area.
- Vaginal skin changes: The inner vaginal lining becomes thinner (atrophic) and may appear paler. The outer skin (vulva) can also become fragile. These changes are part of GSM and are linked to itchiness and soreness. Itching can also accompany redness or small bumps if inflammation develops.
- Other symptoms: Some women notice increased frequency or urgency of urination, or recurrent urinary infections, because the urethra and bladder are also estrogen-sensitive. (This is why the syndrome is “genitourinary.”) Hot flashes and night sweats are separate “vasomotor” symptoms of menopause; though common, they improve over time, whereas vaginal dryness and itching usually need active management.
In summary, vaginal dryness during menopause is very common and often causes itching or burning. If you feel itchy or sore in and around your vagina, or if intercourse is painful, these are classic signs of atrophic vaginitis or GSM.
Effective Vaginal Itching Treatment Options
Good news: there are many proven ways to relieve menopause-related vaginal itch and dryness. Treatment ranges from simple over-the-counter measures to prescription therapies. Key options include:
- Vaginal lubricants and moisturizers: These non-hormonal products add moisture and reduce friction. Water-based or silicone-based lubricants (for example, Astroglide, K-Y Jelly, or similar) can be applied before intercourse to ease dryness and itching during sex. Regular vaginal moisturizers (like Replens or generic polycarbophil gels) are used routinely (several times a week) to maintain moisture and skin health. (Note: avoid scented products or oil-based lubricants if you’re also using latex condoms.) These measures often bring fast symptom relief.
- Vaginal estrogen therapy (topical hormones): Creams, tablets, or rings that release low-dose estrogen in the vagina are the gold-standard treatment for GSM. Such therapy restores moisture, thickens the vaginal lining, and normalizes pH. Compared to oral HRT, vaginal estrogen works in very low doses with minimal absorption into the bloodstream. According to Brigham and Women’s Hospital, local vaginal estrogen is “the most effective treatment for GSM,” rebuilding healthy vaginal tissue and lubrication. (Examples include estradiol or conjugated estrogen creams, Vagifem tablets, or an estrogen ring. Your doctor will advise dosing.) Even in women with a history of breast cancer, a gynecologist may consider carefully supervised local estrogen for severe symptoms.
- Systemic hormone therapy (HRT): If a woman has other menopausal issues (like hot flashes) along with vaginal symptoms, systemic estrogen (pills, patches, or gels) can help both. However, vaginal itching usually responds to local treatment, so systemic therapy isn’t always needed. Always discuss risks and benefits with your doctor.
- Non-hormonal prescription options: For women who cannot or do not want estrogen, alternatives exist. Vaginal DHEA inserts (prasterone) and the pill ospemifene (Osphena) work on estrogen receptors in the vagina to improve symptoms. Over-the-counter remedies like hyaluronic acid gels or vaginal lidocaine (to numb pain) are also used. In one Mayo Clinic study, applying lidocaine jelly before sex relieved pain for some women.
- Other therapies: Some “energy-based” devices (laser or radiofrequency) claim to rejuvenate vaginal tissues. So far, evidence for long-term benefit is limited, and some experts advise caution. You may discuss these with a specialist, but rely primarily on proven treatments.
- Pelvic floor therapy and dilators: In severe atrophy, vaginal dilators (graduated plastic cones) can gently stretch the vagina to combat tightening. Pelvic floor exercises or working with a pelvic therapist can also improve blood flow and tissue health.
No single solution fits everyone. Often, a combination of lubricant use, vaginal estrogen (or other meds), and lifestyle changes gives the best results. A healthcare provider can help tailor a plan.
Remedies and Lifestyle Tips for Relief
In addition to medical treatments, daily habits can ease vaginal itching and support vaginal health:
- Use gentle, fragrance-free products: Avoid soaps, bubble baths, scented lotions, or douches near the vulva – they can worsen dryness and irritation. Instead, clean the area with plain water or a mild, unscented cleanser. The NHS advises using only “unperfumed soaps and washes around your vagina,” and warns not to use products (like body creams) that aren’t meant for vaginal use.
- Stay hydrated and choose breathable fabrics: Drinking enough water and wearing cotton underwear can help keep skin hydrated. Tight, synthetic clothing may trap heat and moisture, aggravating itch. “Cotton undies” and loose clothes can reduce friction.
- Maintain sexual activity or stimulation: Even when libido is low, sexual activity (with lubrication) or vaginal “micro-moisturizing” can improve blood flow to the vaginal area. Medical experts recommend pelvic exercises and arousal time as a natural way to boost moisture. The Menopause Society notes that “regular sexual stimulation promotes vaginal blood flow and secretions,” which helps tissue health.
- Try soothing remedies: Applying a cold (cool) compress or taking a cool sitz bath can relieve acute itching. Some women find relief from an oatmeal (colloidal) bath for irritated skin. Always pat (don’t rub) the area dry afterward and apply an approved vaginal moisturizer.
- Healthy lifestyle: Giving up smoking, cutting back on alcohol, and exercising can all help improve circulation and overall skin health. Eat a healthy diet high in healthy fats (such as omega-3 fatty acids), which help keep the skin plump. Take steps to reduce stress and get plenty of sleep, as overall health can affect menopausal symptoms.
- Avoid scratching: It may be difficult, but it is essential to avoid scratching the skin. Scratching the skin can cause it to tear, worsening itching and irritation. If the itching occurs at night, wearing cotton gloves to bed or applying hydrocortisone cream (1%) for a few days (only if recommended by a pharmacist) may help break the cycle of itching and scratching.
Overall, consistent self-care makes a big difference. Simple measures like daily moisturization, gentle cleansing, and lifestyle tweaks can provide extra comfort alongside any medical treatments you’re using.
When to See a Menopause Doctor or Women’s Health Specialist
If home remedies are not helping with your symptoms, it is time to visit a menopause doctor or women’s health specialist (such as a gynecologist who knows about menopause) if:
- Your itching or dryness has persisted for weeks despite using over-the-counter creams, lubricants, or home remedies.
- You have pain, bleeding, spotting, or abnormal discharge, in addition to itching. (These symptoms may indicate that further evaluation is needed.)
- Your itching or irritation is so bad that it interferes with sleep or daily activities.
According to medical guidelines, any itch or soreness that does not improve with basic care merits a doctor’s visit. The U.S. Office on Women’s Health explicitly advises seeing a provider “if you have vaginal itching or irritation, as it may be a sign of infection.” The Mayo Clinic similarly recommends seeing a doctor if you have burning or soreness in the vagina, or painful sex that doesn’t improve after using lubricants and moisturizers.
A specialist visit can ensure correct diagnosis (ruling out infections or skin conditions) and open the door to prescription options. For example, a menopause specialist can prescribe low-dose vaginal estrogen or other therapies tailored to you. They can also check for other menopause symptoms (like hot flashes, mood changes, or bone health) and create a comprehensive plan. Don’t hesitate to use the term “menopause symptoms” when describing your situation – it helps the provider understand you’re dealing with hormonal effects.
In short, don’t tough it out alone if symptoms are bad. A woman’s health specialist has the expertise to guide you. In fact, the North American Menopause Society advises seeing a certified menopause practitioner (a provider specially trained in menopause) for troublesome symptoms. They can give personalized advice on both medical and lifestyle treatments. Your family doctor can also help, but a dedicated menopause clinic or specialist often has more experience with specific remedies for vaginal health.
How Menopause Clinics (e.g., in London) Can Help
Specialized menopause clinics and doctors are increasingly available to women seeking relief. These clinics offer expert, evidence-based care for menopause, vaginal care, and other symptoms. For example, some large health centers and private practices (including in London) have menopause specialists or certified practitioners on staff. These specialists can evaluate your hormonal status, review treatment options like HRT, and monitor progress over time.
In the UK, there are dedicated services and programs (such as “My Menopause Support“ networks and NHS or private menopause clinics) that focus on midlife women’s health. A menopause clinic visit might include a thorough exam, hormone level testing, and a custom treatment plan. The provider can answer questions about “menopause vaginal symptoms” and prescribe therapies that might not be covered over-the-counter. They can also manage related issues – for instance, recommending skin care tips if menopause skin changes (including vulvar skin) are contributing to itching.

Many clinics offer both in-person and telehealth appointments. In London, for instance, there are well-known menopause treatment centers where experienced doctors help women with relief for menopause vaginal symptoms and other effects. These specialists stay up to date on the latest research and can suggest advanced options (such as compounded bioidentical therapies or pelvic physiotherapy) when needed. They can also coordinate care with pelvic floor therapists or dermatologists if there are complicating factors.
Finally, specialized clinics also offer long-term support. Menopause can be a long process that takes years, so it is always a good idea to have a “menopause doctor” or “women’s health specialist” familiar with your medical history. They can then adjust your treatment as your body changes, ensuring you always maintain a high quality of life.
Sources:
https://www.brighamandwomens.org/obgyn/urogynecology/genitourinary-syndrome-menopause#:~:text=Vaginal%20Symptoms
https://my.clevelandclinic.org/health/diseases/15500-vaginal-atrophy
https://www.nhs.uk/symptoms/vaginal-dryness/#:~:text=Do
https://womenshealth.gov/menopause/menopause-and-sexuality#:~:text=cause%20irritation,be%20a%20sign%20of%20infection
https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288
Frequently Asked Questions
Is vaginal itching a normal symptom of menopause?
Yes. Vaginal itching is a common menopause symptom caused by declining estrogen levels. Lower estrogen makes vaginal tissues thinner, drier, and more sensitive, leading to itching and irritation. This condition is medically known as Genitourinary Syndrome of Menopause (GSM).
Can menopause vaginal itching go away on its own?
In most cases, no. Unlike hot flashes, vaginal dryness and itching tend to worsen over time without treatment. However, symptoms can be effectively managed with vaginal moisturizers, lubricants, or hormone-based therapies recommended by a healthcare provider.
What is the best treatment for menopause-related vaginal itching?
The most effective treatment is low-dose vaginal estrogen therapy, which restores moisture and strengthens vaginal tissue. For women who prefer non-hormonal options, vaginal moisturizers, lubricants, and prescription alternatives like vaginal DHEA may also provide relief.
Are home remedies effective for vaginal itching during menopause?
Mild symptoms may improve with lifestyle changes such as using fragrance-free products, wearing cotton underwear, staying hydrated, and applying vaginal moisturizers regularly. However, persistent or severe itching should be evaluated by a menopause doctor or women’s health specialist.
When should I see a menopause specialist for vaginal itching?
You should see a specialist if itching lasts more than a few weeks, interferes with daily life or sleep, causes pain or bleeding, or does not improve with over-the-counter treatments. A menopause clinic can provide targeted, evidence-based treatment options.
Can vaginal itching during menopause be a sign of infection?
Sometimes. While menopause is a common cause, infections such as yeast or bacterial vaginosis can also cause itching. If symptoms include unusual discharge, odor, or pain, medical evaluation is important to rule out infection.