“Is this normal?” “Am I imagining things?” “Why does no one understand what I’m going through?”
If you’ve found yourself asking these questions, you’re not alone. Every single day, I sit across from women who feel confused, dismissed, and utterly overwhelmed by the changes happening in their bodies. They arrive at my clinic clutching notes, worried they’re losing their minds, convinced something must be seriously wrong.
Let me tell you something I wish every woman knew: what you’re experiencing is real. It’s not “just stress,” it’s not “all in your head,” and it’s certainly not something you should have to endure in silence. Your symptoms are the direct result of profound hormonal shifts, and you absolutely deserve to be taken seriously.
I’m Dr Sonia Dudeja, a certified menopause specialist practising here in the UK, and I’ve dedicated my career to ensuring women’s voices are heard during this transformative time. This comprehensive symptoms checklist is the very first tool I hand to my patients—because naming what’s happening to you is the first powerful step towards reclaiming control of your health.
Why You Need This Checklist Right Now
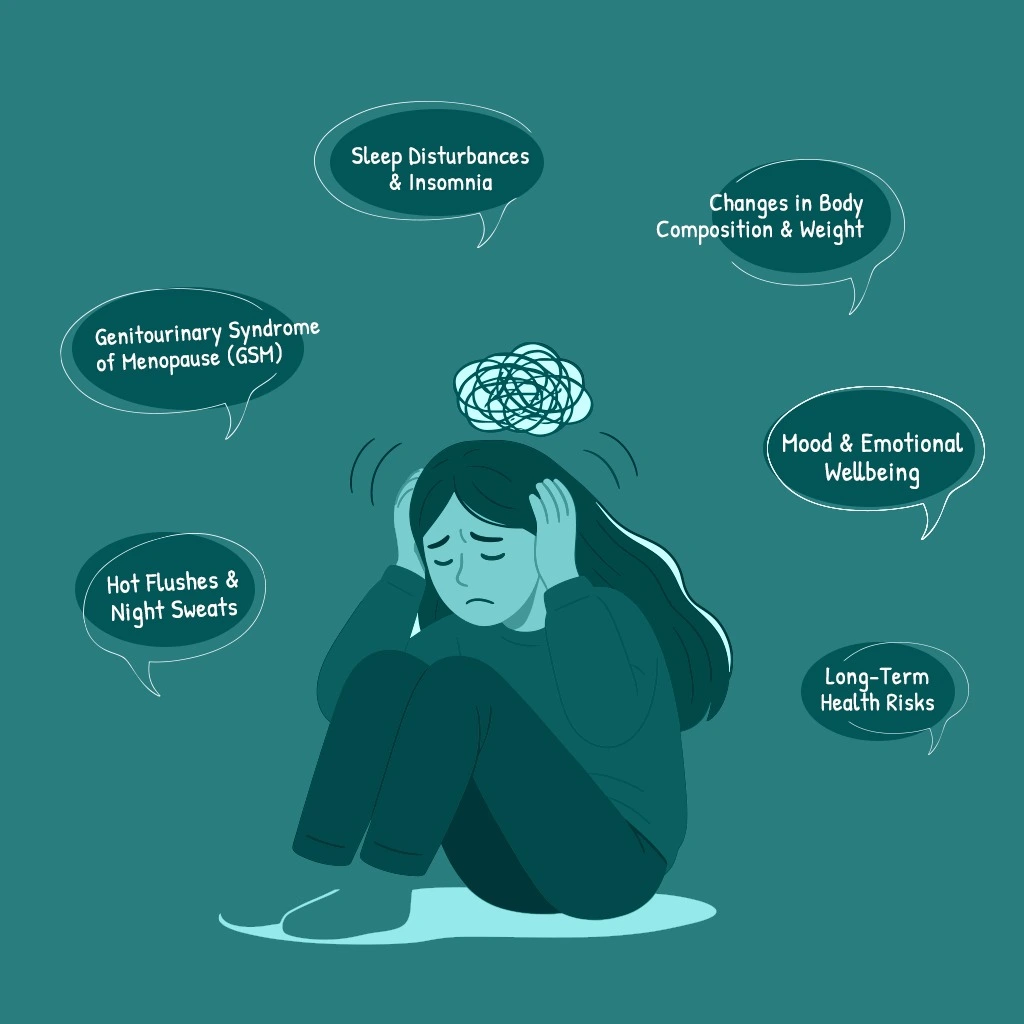
Navigating perimenopause and menopause shouldn’t feel like stumbling through fog. Yet that’s precisely how many women describe it to me. The problem? Fluctuating hormones don’t just affect your periods—they influence nearly every system in your body, creating a bewildering constellation of symptoms that can feel utterly random.
This isn’t a guessing game you should face alone.
Here’s exactly how this checklist will help you:
Identify Clear Patterns – When you see which symptoms cluster together, you begin building an accurate picture of what’s actually happening hormonally. This matters enormously when seeking proper treatment.
Track Your Personal Journey – Documenting the frequency and severity of your experiences gives you objective data, not just vague feelings. This transforms “I feel awful” into “I’ve had severe night sweats 5 nights a week for 3 months.”
Empower Your Medical Consultations – When you walk into your GP’s surgery or specialist appointment with this completed checklist, you provide structured, undeniable evidence of what you’re facing. It ensures precious consultation time focuses on solutions, not lengthy explanations.
This checklist reflects the latest evidence-based guidance, including the updated NICE guideline on menopause (NG23, November 2024) and recommendations from the British Menopause Society, which I use daily in my practice at MyMenopauseSupport.org.
Your Comprehensive Menopause Symptoms Checklist
Mark the symptoms you’re experiencing. Remember—there’s no “typical” menopause journey. Yours is uniquely your own, and that’s exactly as it should be.
🚨 Cycle & Vasomotor Symptoms (Temperature Control)
These are often the very first signs of hormonal fluctuation that prompt women to ring my clinic.
☐ Irregular Periods – Changes in your menstrual flow (becoming heavier or lighter), cycle length varying wildly, or skipping months altogether. This unpredictability can be the most unsettling early sign.
☐ Hot Flushes – Sudden, intense waves of heat flooding through your face, neck, and chest. Research confirms that whilst hot flushes are considered a hallmark menopause symptom, HRT remains the most effective treatment for these vasomotor symptoms. They strike without warning and can leave you drenched and embarrassed in the middle of meetings.
☐ Night Sweats – Severe hot flushes during sleep that soak through your nightclothes and sheets, forcing you to change in the middle of the night and destroying any hope of restful sleep.
☐ Heart Palpitations – A noticeable sensation of your heart racing, fluttering, or pounding. This can be genuinely alarming, especially when it happens suddenly.
🧠 Mood & Emotional Wellbeing
As oestrogen levels decline, they directly impact your brain’s neurotransmitters—particularly serotonin. This isn’t weakness. It’s biochemistry.
☐ Mood Swings – Rapid, unpredictable emotional shifts. You might feel absolutely fine one moment, then inexplicably irritable or tearful the next, leaving you feeling like you’re losing control.
☐ Anxiety – Increased feelings of worry, nervousness, or a persistent sense of dread that feels completely out of character. Many women describe feeling “on edge” constantly.
☐ Irritability – Finding yourself easily annoyed, frustrated, or snapping at loved ones or colleagues over minor things that wouldn’t normally bother you.
☐ Low Mood or Depression – Persistent feelings of sadness, hopelessness, or losing interest in activities and hobbies that once brought you genuine joy. Current guidelines recommend considering HRT to alleviate depressive symptoms that onset around the same time as other menopause-associated symptoms.
☐ Panic Attacks – Sudden, intense episodes of overwhelming fear accompanied by physical symptoms like a racing heart, shortness of breath, or feeling like you’re losing control.
💡 Cognitive Symptoms (“Brain Fog”)
This is hands down one of the most distressing symptoms for the professional women I treat. Let me reassure you immediately: research studies validate that cognitive complaints at menopause are real, with difficulties in learning and verbal memory being especially common, but performance typically remains within normal range for the vast majority of women.
☐ Memory Lapses – Forgetting familiar names, missing appointments you’ve written down, or walking into a room with absolutely no idea why you went there. Studies show that between 31% and 44% of women report forgetfulness during the menopausal transition.
☐ Difficulty Concentrating – Struggling to focus on tasks, finding reading difficult, or losing track of conversations mid-sentence. Work that once felt effortless now requires enormous mental effort.
☐ Mental Confusion – Feeling “fuzzy,” less sharp than usual, or finding your thinking feels disorganised and slow. These cognitive changes emerge in perimenopause when menstrual cycles become irregular, and the timing suggests an aetiology linked to hormones rather than dementia, which is rare at this age.
😴 Sleep & Energy Levels
Sleep disruption creates a vicious cycle—poor sleep worsens mood swings, intensifies brain fog, and compounds fatigue. Breaking this cycle becomes crucial.
☐ Insomnia – Difficulty falling asleep despite feeling utterly exhausted, or lying awake for hours with your mind racing.
☐ Frequent Night Wakings – Waking multiple times throughout the night, often due to temperature changes, anxiety, or for no apparent reason at all.
☐ Chronic Fatigue – A persistent, bone-deep tiredness that sleep doesn’t fix. You wake up feeling as exhausted as when you went to bed.
💪 Physical & Body Changes
Oestrogen receptors exist throughout your entire body—in your joints, muscles, skin, and more. This explains why declining oestrogen creates such widespread physical symptoms, often misattributed to “just getting older.”
☐ Weight Gain – Particularly around your abdomen and midsection, despite eating exactly as you always have. This stubborn belly fat seems to appear overnight and refuses to budge.
☐ Joint & Muscle Pain – Unexplained aches, stiffness, or soreness in your knees, hips, wrists, or shoulders. Many women worry they’re developing arthritis when it’s actually hormonal.
☐ Breast Tenderness – Soreness, swelling, or sensitivity similar to what you might have experienced with PMS, but more unpredictable.
☐ Headaches or Migraines – An increase in frequency or severity of headaches, or developing migraines if you’ve never experienced them before.
☐ Bloating – Persistent feelings of fullness, uncomfortable water retention in your abdomen, or clothes feeling tight around your middle.
☐ Dizziness – Feeling lightheaded, unsteady on your feet, or experiencing brief episodes of vertigo.
❤️ Genitourinary Symptoms (Vaginal & Bladder Health)
These symptoms are collectively known as Genitourinary Syndrome of Menopause (GSM). Without treatment, they often persist and worsen—but here’s the good news: they’re highly manageable with the right approach. Current NICE guidance recommends offering vaginal oestrogen to people with genitourinary symptoms, including those already using systemic HRT.
☐ Vaginal Dryness – Itching, burning, or general discomfort in the vaginal area. This affects daily comfort, not just intimacy.
☐ Low Libido – A noticeable decrease in your desire for sexual activity, which can strain relationships and affect your sense of self.
☐ Painful Intercourse – Discomfort or pain during sex (known medically as dyspareunia), often linked to vaginal dryness and thinning vaginal tissues.
☐ Urinary Incontinence – Leaking small amounts of urine when you cough, sneeze, laugh, or exercise. This can be mortifying and lead to avoiding activities you love.
☐ Urinary Urgency & Frequency – A sudden, overwhelming need to urinate, or finding yourself needing the toilet far more often than usual, including waking multiple times at night.
✨ Skin, Hair & Sensory Changes
☐ Dry or Itchy Skin – Skin that feels noticeably thinner and drier. Some women report a peculiar “crawling” sensation on their skin, medically called formication.
☐ Hair Changes – Thinning hair on your scalp, or noticing more hair in your brush than usual. Sometimes accompanied by unwanted facial hair growth.
☐ Brittle Nails – Nails that crack, split, or break far more easily than they used to.
☐ Changes in Body Odour – Noticing your sweat smells different or stronger than before.
☐ Electric Shock Sensations – Brief, strange feelings like an electric shock under your skin or in your head. Whilst odd, this is a recognised menopause symptom.
☐ Burning Mouth Syndrome – A scalding or tingling sensation on your tongue, lips, or throughout your mouth.
Evidence-Based Treatment Options
Understanding your symptoms is crucial, but knowing effective treatments exist is equally important. The updated NICE guideline emphasises individualised care and shared decision-making when choosing treatments.
Hormone Replacement Therapy (HRT) – Whilst HRT has some risks, current evidence shows it’s unlikely to increase or decrease overall life expectancy. The key is finding the right approach for your individual circumstances.
Cognitive Behavioural Therapy (CBT) – Research now supports menopause-specific CBT as an option for vasomotor symptoms, either alongside HRT or as an alternative for those who cannot or prefer not to take it. It may also improve sleep quality and mood.
Lifestyle Modifications – Regular exercise, stress management, and dietary adjustments all play crucial roles in symptom management.
How to Use This Checklist Before Your Consultation
Simply ticking boxes helps, but I encourage my patients to go further. Here’s how to make this checklist truly work for you:
Rate the Severity – For each symptom you’re experiencing, note whether it’s:
- Mild: Noticeable but doesn’t interfere with your daily life
- Moderate: Interferes with some daily activities or relationships
- Severe: Significantly disrupts your life, work, or wellbeing
Track the Frequency – Note how often each symptom occurs—is it daily, several times weekly, or monthly? Patterns matter enormously.
Bring It With You – This annotated checklist becomes your evidence. It tells your story clearly and comprehensively, ensuring nothing important gets missed during your appointment. It forms the foundation from which we’ll work to establish the root cause of your symptoms and craft your personalised treatment plan.
A Vital Note You Must Know
If you experience any vaginal bleeding after reaching menopause—meaning after 12 consecutive months without a period—you must see your GP or a specialist like myself promptly for investigation. Whilst often benign, post-menopausal bleeding always requires proper medical assessment. This is non-negotiable.
Your Voice Matters. Your Experience is Valid.
Completing this checklist is a powerful act of self-advocacy. It marks the end of your symptoms being minimised, dismissed, or ignored. It signals the beginning of your journey towards effective, evidence-based solutions tailored specifically for you.
Research shows that more than 75% of women experience menopausal symptoms, with a quarter describing their symptoms as severe. You’re far from alone in what you’re facing.
You don’t have to navigate perimenopause or menopause alone, struggling in silence whilst life passes you by. I’m here to listen without judgement, to validate what you’re experiencing, and to provide the expert, compassionate care you absolutely deserve.
Every woman’s menopause journey is different, but you shouldn’t have to figure yours out through trial and error, feeling dismissed by healthcare providers who don’t specialise in this area.
Ready to take the next step? Book a consultation with me today at MyMenopauseSupport.org, and let’s use your completed checklist as the roadmap to guide us towards your wellbeing, your confidence, and your quality of life.
You deserve to feel like yourself again. Let’s make that happen together.
Dr Sonia Dudeja
Certified Menopause Specialist
Founder, MyMenopauseSupport.org
References
This article is based on the latest evidence-based guidelines including:
- NICE Guideline NG23: Menopause – Identification and Management (updated November 2024)
- British Menopause Society clinical guidance and consensus statements
- Joint position statement by the British Menopause Society, Royal College of Obstetricians and Gynaecologists, and Society for Endocrinology (2022)
- Peer-reviewed research on cognitive function during menopause, including studies published in Climacteric and Post Reproductive Health